HIPAA Compliance in 2025: Avoid Costly IT Mistakes
🎙️ Dive Deeper with Our Podcast!
HIPAA Compliance 2025: IT Security and Violation Avoidance
Quick Summary
Healthcare organizations face unprecedented cybersecurity challenges in 2025, with HIPAA violations costing an average of $1.5 million per incident. This comprehensive guide covers the most common IT mistakes that lead to costly penalties, including inadequate risk assessments, weak access controls, unencrypted data, and outdated systems. Learn essential best practices for healthcare IT security, access a complete HIPAA audit checklist, and discover how to build a culture of compliance that protects patient data and your organization’s reputation. Whether you’re a small practice or large healthcare system, understanding these critical compliance requirements is essential for avoiding violations and maintaining patient trust in today’s digital healthcare environment.
The healthcare industry faces mounting pressure to protect patient data while navigating an increasingly complex digital landscape. As we move through 2025, HIPAA compliance 2025 requirements have become more stringent, and the consequences of non-compliance more severe. Healthcare organizations that fail to prioritize healthcare IT security face average penalties exceeding $1.5 million per violation, not to mention the irreparable damage to patient trust and organizational reputation.
Understanding the latest compliance requirements and implementing robust security measures is no longer optional—it’s essential for survival in today’s healthcare environment.
The Evolving Landscape of HIPAA Compliance in 2025
Healthcare organizations now operate in an environment where cyber threats are more sophisticated than ever before. The shift to telehealth, cloud-based systems, and interconnected medical devices has expanded the attack surface exponentially. Recent data breaches affecting millions of patients have prompted regulators to intensify their scrutiny of healthcare IT security practices.
The Office for Civil Rights (OCR) has signaled that 2025 will see increased enforcement actions, particularly targeting organizations that demonstrate willful negligence or repeated violations. This means that reactive approaches to compliance are no longer sufficient—healthcare providers must adopt proactive strategies that anticipate risks before they materialize.
Common IT Mistakes That Lead to HIPAA Violations
Inadequate Risk Assessment Protocols
Many healthcare organizations conduct risk assessments as a checkbox exercise rather than a comprehensive evaluation of their security posture. This superficial approach leaves vulnerabilities undetected and creates a false sense of security. Effective risk assessments should be ongoing processes that account for new technologies, changing workflows, and emerging threats.
Insufficient Employee Training and Awareness
Human error remains the leading cause of data breaches in healthcare settings. When staff members lack proper training on HIPAA compliance 2025 requirements, they inadvertently create security gaps. Common mistakes include sharing passwords, accessing patient records without authorization, and falling victim to phishing attacks.
Weak Access Controls and Authentication
Implementing proper access controls is fundamental to healthcare IT security, yet many organizations still rely on outdated authentication methods. Single-factor authentication, shared credentials, and excessive user privileges create unnecessary risks. Modern compliance requires multi-factor authentication, role-based access controls, and regular access reviews.
Unencrypted Data Storage and Transmission
Encryption is a critical safeguard for protected health information (PHI), yet some organizations still transmit or store data without adequate encryption. This oversight can transform a minor security incident into a reportable breach. Both data at rest and data in transit must be encrypted using industry-standard protocols.
Outdated Software and Unpatched Systems
Running outdated software with known vulnerabilities is one of the most preventable IT mistakes in healthcare. Legacy systems that no longer receive security updates pose significant risks. Organizations must maintain current versions of all software and implement robust patch management processes.
Lack of Business Associate Agreements
Healthcare organizations frequently work with third-party vendors who have access to PHI. Without properly executed Business Associate Agreements (BAAs), organizations remain liable for their vendors’ security failures. Every entity with access to PHI must have a compliant BAA in place.
Inadequate Incident Response Planning
When breaches occur, the lack of a comprehensive incident response plan can amplify damage and increase penalties. Organizations must be able to detect breaches quickly, contain them effectively, and report them within the required 60-day window.
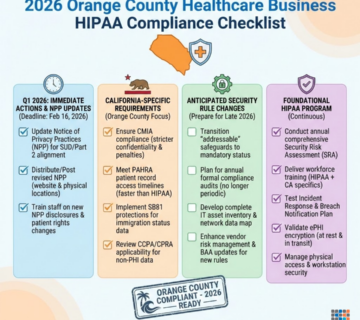
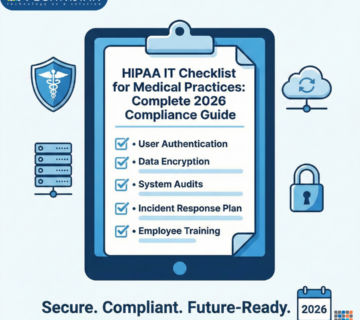
Building a Comprehensive HIPAA Audit Checklist
Creating a robust HIPAA audit checklist helps organizations maintain continuous compliance and identify vulnerabilities before they become violations. Your checklist should address all aspects of the HIPAA Security Rule.
Administrative Safeguards
Your administrative safeguards form the foundation of your compliance program. Begin by designating a qualified security officer responsible for developing and implementing security policies. Conduct thorough risk analyses at least annually and whenever significant changes occur to your IT infrastructure. Implement workforce security procedures that include authorization protocols and supervision of staff with access to PHI.
Establish clear policies for information access management, ensuring employees can only access PHI necessary for their job functions. Develop comprehensive security awareness training programs that cover current threats and best practices. Create and test incident response procedures to ensure your team can respond effectively to security events.
Physical Safeguards
Physical security often receives insufficient attention in healthcare IT security planning. Implement facility access controls that restrict physical access to electronic information systems and the facilities housing them. Install workstation security measures that specify proper workstation functions and physical attributes. Develop device and media controls that govern the receipt, removal, and disposal of electronic media containing PHI.
Technical Safeguards
Technical safeguards represent the technology-based protections for your electronic PHI. Implement robust access control mechanisms including unique user identification, emergency access procedures, automatic logoff, and encryption where appropriate. Deploy comprehensive audit controls that record and examine system activity. Ensure the integrity of electronic PHI through mechanisms that protect data from improper alteration or destruction.
Implement person or entity authentication procedures to verify that individuals or systems seeking access to PHI are who they claim to be. Apply transmission security measures including encryption and integrity controls for PHI transmitted over electronic networks.
Best Practices for Healthcare IT Security in 2025
Embrace Zero Trust Architecture
Traditional perimeter-based security models no longer provide adequate protection. Zero trust architecture assumes no user or device should be trusted by default, regardless of location. This approach requires continuous verification of all users and devices attempting to access your systems.
Implement Advanced Threat Detection
Modern threats require sophisticated detection capabilities. Deploy security information and event management (SIEM) systems that aggregate logs from across your infrastructure and use artificial intelligence to identify suspicious patterns. Consider managed detection and response services if your organization lacks the in-house expertise to monitor systems continuously.
Regular Penetration Testing and Vulnerability Assessments
Finding vulnerabilities before attackers take advantage of them is made easier with proactive security testing. Conduct regular penetration testing by qualified professionals who can simulate real-world attacks against your systems. Perform vulnerability assessments quarterly or after significant infrastructure changes.
Secure Cloud Implementations
As healthcare organizations increasingly adopt cloud services, ensuring HIPAA compliance 2025 requirements in cloud environments becomes critical. Work only with cloud service providers who offer HIPAA-compliant infrastructure and sign BAAs. Implement proper configuration management to prevent common cloud security mistakes like exposed storage buckets or misconfigured access controls.
Mobile Device Management
The proliferation of mobile devices in healthcare settings introduces new security challenges. Implement comprehensive mobile device management solutions that can enforce security policies, enable remote wiping of lost devices, and ensure devices accessing PHI meet security requirements.
The True Cost of Non-Compliance
HIPAA violations carry severe financial and reputational consequences. Financial penalties range from $100 to $50,000 per violation, with annual maximums reaching $1.5 million per violation category. Recent enforcement actions have resulted in multi-million dollar settlements, demonstrating regulators’ willingness to impose significant penalties.
Beyond direct financial penalties, organizations face substantial costs from breach remediation, legal fees, credit monitoring services for affected patients, and increased insurance premiums. The reputational damage can be even more devastating, leading to patient attrition, difficulty attracting new patients, and challenges recruiting qualified staff.
In severe cases, organizations may face criminal charges resulting in imprisonment for individuals responsible for the violations. The Department of Justice has increased prosecutions for HIPAA violations, particularly in cases involving intentional disclosure or obtaining of PHI.
Preparing for HIPAA Audits
The OCR conducts both random audits and investigations triggered by complaints or breaches. Preparation is essential for demonstrating compliance and avoiding penalties.
Maintain comprehensive documentation of all security policies, procedures, training sessions, risk assessments, and incident responses. Documentation serves as evidence of your good faith efforts to maintain compliance. Conduct regular internal audits using your HIPAA audit checklist to identify and remediate issues before external auditors discover them.
Designate a compliance team responsible for coordinating audit responses and maintaining documentation. This team should understand all aspects of your security program and can quickly provide requested information to auditors. Consider conducting mock audits with external consultants who can provide objective assessments of your compliance posture and identify gaps in your program.
Emerging Technologies and HIPAA Compliance
Artificial Intelligence and Machine Learning
Healthcare organizations increasingly leverage AI and machine learning for diagnostics, treatment planning, and administrative functions. These technologies introduce unique compliance challenges. Ensure AI systems processing PHI maintain appropriate security controls and that algorithms don’t create unintended privacy risks through pattern recognition or data aggregation.
Internet of Medical Things (IoMT)
Connected medical devices improve patient care but expand your organization’s attack surface. Each IoMT device represents a potential entry point for attackers. Implement network segmentation to isolate medical devices, maintain updated device inventories, and work with manufacturers who prioritize security in their device designs.
Blockchain in Healthcare
Some organizations explore blockchain technology for secure health information exchange. While blockchain offers promising security features, implementation must still meet all HIPAA requirements. Carefully evaluate how blockchain solutions handle patient rights, including the right to amend records and request accounting of disclosures.
Creating a Culture of Compliance
Technology alone cannot ensure HIPAA compliance—organizational culture plays a crucial role. Leadership must demonstrate commitment to compliance through resource allocation, policy development, and accountability. When executives prioritize security, employees understand its importance.
Encourage staff to report potential security incidents without fear of punishment. Many breaches worsen because employees fear reporting mistakes. Foster an environment where reporting is viewed as responsible behavior that protects patients rather than an admission of failure.
Integrate security considerations into all decision-making processes. When evaluating new technologies, workflows, or partnerships, security and compliance should be primary considerations rather than afterthoughts. This proactive approach prevents costly retrofitting of security measures.
Frequently Asked Questions
What are the most common HIPAA violations in 2025?
The most frequent violations include unauthorized access to patient records by employees, lack of encryption for electronic PHI, inadequate risk assessments, missing Business Associate Agreements, and failure to provide breach notifications within required timeframes. Phishing attacks leading to compromised credentials also remain a leading cause of breaches.
How often should we conduct HIPAA risk assessments?
Organizations should conduct comprehensive risk assessments at least annually. However, you should also perform assessments whenever significant changes occur, such as implementing new technology, changing business processes, or expanding service offerings. Continuous risk monitoring throughout the year provides the most effective protection.
What is the penalty for HIPAA violations in 2025?
Penalties vary based on the violation’s nature and severity. Tier 1 violations (unknowing) carry penalties of $100-$50,000 per violation. Tier 2 (reasonable cause) ranges from $1,000-$50,000. Tier 3 (willful neglect corrected) ranges from $10,000-$50,000. Tier 4 (willful neglect not corrected) carries penalties of $50,000 per violation. Annual maximums per violation category can reach $1.5 million.
Do small healthcare practices need to comply with HIPAA?
Yes, HIPAA compliance requirements apply to all covered entities regardless of size. This includes individual practitioners, small clinics, and large hospital systems. While smaller practices may have simpler compliance programs, they must still implement appropriate administrative, physical, and technical safeguards to protect PHI.
What should we do if we discover a potential data breach?
Act immediately upon discovering a potential breach. Activate your incident response plan, contain the breach to prevent further unauthorized access, conduct a thorough investigation to determine the scope and cause, and document all actions taken. If the breach affects 500 or more individuals, notify the OCR within 60 days. Breaches affecting fewer individuals must be reported annually.
Are cloud services HIPAA compliant?
Cloud services can be HIPAA compliant if properly configured and managed. The cloud provider must be willing to sign a Business Associate Agreement and offer appropriate security controls. However, ultimate responsibility for compliance remains with the covered entity. You must ensure proper configuration, access controls, and monitoring of your cloud environment.
How long should we retain HIPAA documentation?
HIPAA requires retaining documentation for at least six years from the date of creation or when it was last in effect, whichever is later. This includes policies, procedures, training records, risk assessments, and incident reports. Some state laws may require longer retention periods.
What is the difference between the HIPAA Privacy Rule and Security Rule?
The Privacy Rule establishes national standards for protecting patient health information and governs how PHI can be used and disclosed. The Security Rule specifically addresses electronic PHI (ePHI) and requires administrative, physical, and technical safeguards to ensure its confidentiality, integrity, and availability. Healthcare organizations must comply with both rules.
How Technijian Can Help
Navigating HIPAA compliance 2025 requirements requires specialized expertise and ongoing vigilance. Technijian provides comprehensive HIPAA and healthcare IT compliance services designed to protect your organization from costly violations while enabling you to focus on patient care.
Our experienced team conducts thorough compliance assessments using our proven HIPAA audit checklist, identifying vulnerabilities in your current security posture and providing actionable remediation plans. We understand that every healthcare organization faces unique challenges, which is why we tailor our solutions to your specific environment, size, and risk profile.
Technijian offers complete healthcare IT security services including risk assessments, security awareness training, incident response planning, and continuous monitoring. Our experts stay current with evolving regulations and emerging threats, ensuring your compliance program adapts to the changing landscape. We implement robust technical safeguards including encryption, access controls, audit logging, and network security measures that meet or exceed HIPAA requirements.
Beyond initial compliance, Technijian provides ongoing support to maintain your security posture. We conduct regular reviews, update policies and procedures as regulations change, and help you respond effectively to security incidents. Our proactive approach prevents violations before they occur, protecting your organization from penalties and reputational damage.
Working with Technijian means partnering with a team that understands both the technical and regulatory aspects of healthcare IT security. We translate complex requirements into practical solutions that integrate seamlessly with your operations. Our goal is to make compliance manageable and effective, giving you confidence that your patient data remains secure and your organization stays protected.
Take Action Now
Don’t wait for a breach or audit to discover compliance gaps in your organization. The cost of non-compliance far exceeds the investment in proper security measures. Every day without comprehensive HIPAA compliance puts your organization at risk of penalties, breaches, and reputational damage.
Request a HIPAA compliance review from Technijian today. Our experts will assess your current security posture, identify vulnerabilities, and provide a clear roadmap for achieving and maintaining compliance. Protect your patients, your organization, and your future with comprehensive healthcare IT security solutions designed for 2025 and beyond.
Contact Technijian now to schedule your confidential compliance review and take the first step toward complete HIPAA compliance.
About Technijian
Technijian is a leading provider of comprehensive IT solutions and cybersecurity services, specializing in healthcare technology and HIPAA compliance. With years of experience serving healthcare organizations of all sizes, we understand the unique challenges faced by medical practices, clinics, hospitals, and healthcare service providers in today’s digital landscape.
Our team of certified IT professionals and compliance experts is dedicated to protecting your sensitive patient data while ensuring your technology infrastructure supports efficient healthcare delivery. We combine deep technical expertise with extensive knowledge of healthcare regulations to deliver solutions that not only meet compliance requirements but also enhance operational efficiency.
At Technijian, we believe that robust security and seamless technology should go hand in hand. Whether you need a complete compliance overhaul, ongoing managed IT services, or strategic technology consulting, we provide personalized solutions tailored to your organization’s specific needs and budget. Our proactive approach keeps your systems secure, your data protected, and your practice running smoothly, allowing you to focus on what matters most—providing exceptional patient care.
Trust Technijian to be your partner in healthcare IT excellence and HIPAA compliance.