HIPAA Compliance in 2025: Secure AI and Data Workflows for Healthcare Providers
🎙️ Dive Deeper with Our Podcast!
AI, Cloud, and the Future of HIPAA Compliance
Healthcare providers face an increasingly complex challenge: leveraging powerful AI tools and cloud technologies while maintaining strict HIPAA compliance. As digital transformation accelerates across the medical industry, understanding how to secure patient data within modern IT workflows has never been more critical.
The New Reality of Healthcare IT in 2025
Medical practices, hospitals, and healthcare organizations are rapidly adopting AI-powered diagnostics, cloud-based virtual desktop infrastructure (VDI), and automated administrative workflows. While these technologies promise improved patient outcomes and operational efficiency, they also introduce new compliance vulnerabilities that traditional HIPAA frameworks weren’t designed to address.
The consequences of non-compliance have become more severe. Recent enforcement actions have resulted in multi-million dollar settlements, and the Office for Civil Rights (OCR) has made it clear that ignorance of how new technologies handle Protected Health Information (PHI) is not an acceptable defense.
This guide walks you through maintaining bulletproof HIPAA compliance while embracing the AI and automation tools that modern healthcare demands.
Understanding HIPAA Compliance in the AI Era
HIPAA compliance in 2025 extends far beyond locked file cabinets and encrypted email. The fundamental requirements remain consistent—protecting the confidentiality, integrity, and availability of PHI—but the attack surface has expanded exponentially.
Core HIPAA Requirements That Haven’t Changed
The Privacy Rule, Security Rule, and Breach Notification Rule still form the foundation of healthcare data protection. Your organization must implement administrative, physical, and technical safeguards regardless of which technologies you deploy. Every system that touches PHI requires a thorough risk assessment, documented policies, and Business Associate Agreements (BAAs) with vendors.
What’s Different About AI in Healthcare IT
Artificial intelligence introduces unique compliance challenges. Machine learning models require training data, which often includes PHI. AI tools may send data to external servers for processing. Large language models might inadvertently memorize sensitive information from training datasets. Automated decision-making systems create new documentation requirements under HIPAA’s accountability provisions.
The critical question becomes: How do you harness AI’s diagnostic and administrative power without exposing patient data to unauthorized access or creating compliance gaps?
HIPAA-Compliant AI Implementation Strategies
Successfully integrating AI into your healthcare workflows requires a compliance-first approach that doesn’t sacrifice innovation.
Selecting AI Tools with HIPAA Compliance Built In
Not all AI platforms are created equal from a compliance perspective. Before implementing any AI solution, verify that the vendor will sign a comprehensive BAA. This legally binding agreement ensures they accept responsibility for protecting PHI that passes through their systems.
Look for AI tools specifically designed for healthcare environments. These solutions typically include PHI redaction capabilities, on-premises deployment options, or private cloud instances that never expose data to shared infrastructure. Vendors should provide detailed documentation of their security controls, encryption standards, and audit capabilities.
Generic AI platforms like ChatGPT, Claude, or other consumer-grade large language models should never receive actual PHI without explicit HIPAA-compliant configurations. Many healthcare organizations create sandboxed AI environments where data is de-identified before processing, maintaining the utility of AI analysis while protecting patient privacy.
Data Minimization and De-identification Techniques
One of the most effective HIPAA compliance strategies involves limiting how much PHI reaches AI systems in the first place. Data minimization principles suggest using only the minimum necessary information for each task.
For AI training datasets, proper de-identification removes the 18 HIPAA identifiers that make information individually identifiable. Advanced techniques include data masking, tokenization, and synthetic data generation that preserves statistical relationships without exposing real patient information.
When AI tools absolutely require access to PHI—such as diagnostic imaging analysis—implement technical controls that prevent data retention. Configure systems to process information in memory without creating persistent copies, and establish automated deletion policies that remove temporary files immediately after processing.
Access Controls and Audit Trails
HIPAA’s Security Rule mandates that only authorized individuals access PHI. For AI systems, this means implementing role-based access controls that restrict who can deploy models, access training data, or review AI-generated insights.
Every interaction with PHI must be logged and auditable. Your AI infrastructure should capture detailed records showing who accessed what data, when they accessed it, what actions they performed, and the business justification for that access. These audit logs become critical during compliance reviews and breach investigations.
Modern healthcare IT environments benefit from centralized identity and access management (IAM) solutions that provide single sign-on across AI tools, electronic health records, and administrative systems while maintaining granular permission controls and comprehensive activity monitoring.
Cloud VDI and HIPAA Compliance
Virtual Desktop Infrastructure has become the backbone of modern healthcare IT, enabling secure remote access and centralized data management. However, moving desktops to the cloud introduces specific HIPAA considerations.
Choosing HIPAA-Compliant Cloud Providers
Major cloud platforms like Microsoft Azure, Amazon Web Services, and Google Cloud all offer HIPAA-compliant services, but compliance isn’t automatic. You must specifically select HIPAA-eligible services, configure them correctly, and maintain a signed BAA with your cloud provider.
Understanding the shared responsibility model is essential. Cloud providers secure the underlying infrastructure, but you remain responsible for properly configuring security settings, managing access controls, encrypting data, and monitoring for threats. A misconfigured cloud environment—even on a compliant platform—creates HIPAA violations that fall entirely on your organization.
Securing Virtual Desktop Environments
Cloud VDI solutions should enforce encryption both in transit and at rest. All connections between end-user devices and cloud desktops must use secure protocols that prevent interception. The virtual desktops themselves should be configured to prevent data from being downloaded to unmanaged personal devices.
Session recording and monitoring capabilities help demonstrate HIPAA compliance by documenting exactly what users do with PHI. However, these same capabilities require careful configuration to avoid creating excessive copies of sensitive data that expand your compliance obligations.
Multi-factor authentication becomes non-negotiable for cloud VDI access. Username and password combinations alone provide insufficient protection for systems containing PHI. Implement hardware tokens, biometric authentication, or push-based verification to ensure that compromised credentials alone cannot grant access to your virtual desktop environment.
Network Segmentation and Zero Trust Architecture
Modern HIPAA-compliant cloud environments implement zero trust principles that assume no user or system should be trusted by default. Network segmentation isolates PHI-containing systems from general corporate infrastructure, limiting the blast radius if a security incident occurs.
Microsegmentation takes this further by creating security boundaries around individual workloads and applications. In a cloud VDI environment, this means that even if an attacker compromises one virtual desktop, they cannot automatically pivot to accessing other systems or datasets.
Continuous monitoring and behavioral analysis help detect anomalous activity that might indicate a breach. AI-powered security tools can identify unusual access patterns, data exfiltration attempts, or compromised credentials in real time, enabling rapid response before significant PHI exposure occurs.
Automation and Workflow Security
Administrative automation promises significant efficiency gains for healthcare providers, but automated workflows that touch PHI require careful security design.
Secure RPA and Workflow Automation
Robotic Process Automation (RPA) tools can handle repetitive tasks like claims processing, appointment scheduling, and medical record updates. From a HIPAA perspective, these automation tools become the electronic equivalent of human users and must be secured accordingly.
Service accounts used by automation tools need unique credentials, appropriate permission levels, and regular password rotation. The principle of least privilege applies—automation should only access the specific data and systems required for its designated tasks.
Automation scripts and configurations should be version-controlled, code-reviewed, and tested in non-production environments before deployment. A poorly written automation script could accidentally expose PHI, process data incorrectly, or create compliance gaps that aren’t discovered until an audit or breach occurs.
API Security for Healthcare Data Integration
Modern healthcare workflows rely on APIs connecting electronic health records, laboratory systems, billing platforms, and specialty applications. Each API endpoint that transmits PHI must implement authentication, authorization, encryption, and rate limiting.
OAuth 2.0 and other modern authentication standards provide more secure alternatives to embedded credentials or API keys. Certificate-based authentication offers even stronger security for server-to-server communication.
API gateways provide centralized security enforcement, logging, and traffic management. They act as a security checkpoint ensuring that all API calls meet HIPAA requirements before reaching backend systems containing PHI.
Automated Compliance Monitoring
Ironically, automation itself provides powerful tools for maintaining HIPAA compliance. Automated security scanning can continuously check for misconfigurations, missing patches, excessive permissions, or policy violations across your entire IT infrastructure.
Compliance automation platforms compare your current configuration against HIPAA requirements and industry benchmarks, generating remediation guidance for identified gaps. This shifts compliance from an annual checklist exercise to an ongoing operational discipline.
Automated incident response playbooks can immediately contain suspected breaches, preserve forensic evidence, and initiate notification procedures when security events exceed predefined thresholds. This rapid response capability significantly reduces the potential impact of security incidents involving PHI.
Employee Training and Security Awareness
Technology alone cannot ensure HIPAA compliance. Your workforce remains the first line of defense against data breaches and the most common source of compliance violations.
Comprehensive HIPAA Training Programs
Every employee with potential PHI access requires regular HIPAA training that covers not just regulations but practical security behaviors. Training should specifically address the AI tools, cloud systems, and automated workflows your organization actually uses.
Role-specific training provides more value than generic compliance courses. Clinical staff need different guidance than IT administrators or billing specialists. Scenario-based training that presents realistic situations helps employees understand how HIPAA principles apply to their daily work.
Documentation of training completion becomes critical during compliance audits. Maintain detailed records showing who received training, when they completed it, what topics were covered, and their assessment results.
Phishing and Social Engineering Defense
Healthcare organizations face relentless phishing campaigns attempting to steal credentials or trick employees into revealing PHI. Regular simulated phishing exercises help employees recognize suspicious messages and report them appropriately.
Security awareness should extend beyond email to include phone-based attacks, physical security tailgating, and manipulation tactics that exploit helpful healthcare workers’ desire to assist patients.
Incident Response Procedures
When security incidents occur—and they will—employees need clear procedures for reporting, escalation, and response. Defining these processes in advance and practicing them through tabletop exercises ensures your team can respond effectively under pressure.
Incident response plans should specifically address AI system failures, cloud service disruptions, automation errors, and other technology-specific scenarios relevant to your modern healthcare IT environment.
Business Associate Agreements in the Modern Healthcare Ecosystem
The expansion of healthcare technology has dramatically increased the number of Business Associates that require formal agreements.
Identifying All Business Associates
Any vendor that creates, receives, maintains, or transmits PHI on your behalf qualifies as a Business Associate under HIPAA. This includes obvious partners like cloud hosting providers and medical transcription services, but also extends to AI platform vendors, analytics services, backup solutions, IT support contractors, and even email hosting providers.
The shift to cloud and AI services means many healthcare organizations now maintain dozens or even hundreds of BAAs. Tracking these agreements, ensuring they contain required provisions, and monitoring Business Associate compliance has become a significant administrative challenge.
Essential BAA Provisions for AI and Cloud Services
Business Associate Agreements must specifically address how the vendor will protect PHI, what security measures they implement, how they’ll report breaches, and their responsibilities if they violate HIPAA requirements.
For AI and cloud services, BAAs should explicitly prohibit using your PHI for training models that benefit other customers, require deletion of PHI after service termination, and specify data location to address multi-jurisdictional regulatory requirements.
Subcontractor provisions ensure that Business Associates cannot delegate your data to third parties without appropriate protections. Given the complex supply chains behind modern cloud and AI services, understanding who actually processes your PHI becomes critical.
Ongoing Business Associate Management
Signing a BAA represents the beginning of your compliance responsibility, not the end. Regular Business Associate assessments verify that vendors maintain the security measures they promised and remain financially viable.
Security questionnaires, third-party audits, and site visits provide insight into Business Associate practices. For critical vendors—those handling large volumes of PHI or providing essential services—annual reassessments should be standard practice.
Contract provisions should include the right to audit Business Associates, receive security reports, and terminate agreements if compliance failures occur. These contractual protections become your primary recourse if a Business Associate’s security failure compromises your patients’ data.
Risk Assessment and Management
HIPAA requires regular risk assessments that identify threats to PHI and implement appropriate safeguards. The addition of AI and cloud technologies fundamentally changes your risk profile.
Conducting Comprehensive Risk Assessments
Effective HIPAA risk assessments inventory all systems containing PHI, identify potential threats to confidentiality, integrity, and availability, evaluate existing security measures, determine likelihood and impact of potential breaches, and document remediation plans for identified gaps.
For AI systems, assess risks associated with data used for model training, potential bias in algorithmic decisions, model failures or unexpected outputs, and third-party AI service dependencies.
Cloud environments require evaluation of provider security practices, configuration management procedures, access control implementations, and business continuity preparations.
Remediation Planning and Implementation
Risk assessments only provide value if you act on their findings. Prioritize remediation based on likelihood and potential impact, addressing the most critical vulnerabilities first.
Document your risk acceptance decisions for vulnerabilities you choose not to immediately remediate. HIPAA doesn’t require perfect security—it requires reasonable and appropriate safeguards based on your organization’s size, complexity, and resources.
Regular reassessment ensures your security posture keeps pace with evolving threats and changing technology. The AI tools and cloud configurations you assessed six months ago have likely changed, introducing new risks that require fresh evaluation.
Breach Prevention and Response
Despite best efforts, breaches can still occur. Preparation significantly reduces their impact and demonstrates HIPAA compliance commitment.
Preventing Common Breach Scenarios
The majority of healthcare data breaches result from preventable causes like unencrypted devices, misaddressed emails, unauthorized access by employees, phishing attacks, ransomware, and misconfigured cloud storage.
Technical controls like device encryption, email security gateways, access monitoring, security awareness training, endpoint protection, and automated configuration management address these common scenarios.
Breach Detection Capabilities
Early breach detection limits PHI exposure and reduces notification obligations. Security information and event management (SIEM) systems aggregate logs from across your IT environment, identifying suspicious patterns that might indicate compromise.
User and entity behavior analytics (UEBA) establish baselines for normal activity and flag deviations. A user suddenly accessing hundreds of patient records, downloading large datasets, or connecting from unusual locations triggers investigation.
For AI and automation systems, implement monitoring that detects data exfiltration attempts, unusual API call patterns, or changes to model behavior that might indicate compromise.
Breach Response Procedures
When a breach is identified, documented procedures ensure consistent response. Immediate containment limits further exposure. Forensic investigation determines the breach’s scope—what PHI was accessed, by whom, and for how long.
HIPAA’s Breach Notification Rule requires notifying affected individuals within 60 days for breaches involving more than 500 people, with simultaneous notification to HHS and potentially media outlets. Smaller breaches require annual reporting. State laws may impose additional notification requirements.
Your breach response plan should pre-identify the response team, define communication protocols, establish notification templates, and outline remediation steps to prevent recurrence.
Ongoing Compliance and Audit Readiness
HIPAA compliance is not a one-time achievement but an ongoing operational discipline that requires continuous attention.
Documentation Requirements
Comprehensive documentation demonstrates compliance during audits and investigations. Maintain written policies covering all HIPAA requirements, risk assessment reports and remediation plans, training records, BAAs with all Business Associates, incident response documentation, and system configuration records.
For AI and automation systems, document what models you deploy, what data they access, how decisions are made, and who oversees their operation. This documentation becomes crucial if algorithmic decisions are questioned or if systems malfunction.
Internal Audit Programs
Regular internal audits identify compliance gaps before external auditors or regulators discover them. Review access logs for unauthorized PHI access, verify employee training completion, confirm BAA coverage for all vendors, test backup and disaster recovery procedures, and assess security control effectiveness.
Self-auditing also demonstrates good faith efforts to maintain compliance, potentially reducing penalties if violations are discovered.
Staying Current with Regulatory Changes
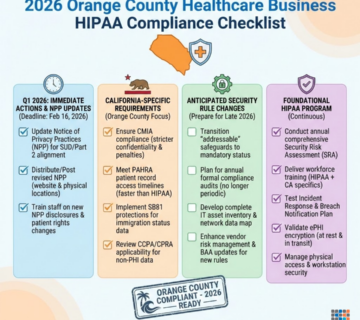
Healthcare regulations continue evolving. The OCR regularly releases guidance addressing new technologies and compliance questions. State laws introduce additional requirements. Court decisions clarify HIPAA’s application to specific scenarios.
Designating a compliance officer or engaging specialized healthcare IT consultants ensures your organization stays informed about regulatory changes affecting your technology deployments.
Frequently Asked Questions
Can we use ChatGPT or other public AI tools for healthcare administrative tasks?
Generic public AI platforms should never receive actual PHI unless they’re specifically configured with HIPAA-compliant enterprise agreements. Most consumer AI services explicitly prohibit submitting sensitive health information in their terms of service. For legitimate healthcare AI use, select platforms that offer BAAs and HIPAA-compliant deployments, often requiring enterprise accounts with additional security features and private hosting.
Are Microsoft 365 and Google Workspace automatically HIPAA compliant?
No. While both Microsoft and Google offer HIPAA-compliant versions of their productivity suites, compliance requires specific configurations and signed Business Associate Agreements. The standard consumer and many business tiers don’t include necessary safeguards. You must actively enable HIPAA-compliant features, configure appropriate security settings, and maintain documentation of these implementations.
How should we handle AI model training that requires patient data?
Use properly de-identified datasets whenever possible, removing all 18 HIPAA identifiers before training. If models absolutely require identifiable information, implement strict access controls, sign BAAs with AI platform vendors, document business justification and safeguards, and conduct thorough risk assessments. Consider using synthetic data generation techniques that create realistic training datasets without actual patient information.
What’s required for HIPAA-compliant remote work with cloud VDI?
Remote access to PHI through cloud VDI requires encrypted connections using VPN or similar secure protocols, multi-factor authentication for all users, endpoint security on devices accessing VDI, session monitoring and recording capabilities, and policies prohibiting data downloads to personal devices. The virtual desktop environment itself must be hosted by HIPAA-compliant cloud providers with appropriate BAAs.
How long do we need to keep HIPAA compliance documentation?
HIPAA requires maintaining documentation for six years from creation date or last effective date, whichever is later. This includes policies, risk assessments, training records, and incident reports. Some state laws impose longer retention requirements. Given the critical nature of compliance documentation, many organizations maintain records indefinitely unless storage constraints require deletion.
Do we need separate risk assessments for each AI tool we implement?
Yes. Each new system, application, or service that creates, receives, maintains, or transmits PHI requires risk assessment addressing its specific vulnerabilities and safeguards. While you can use standardized assessment frameworks, the unique characteristics of each AI tool—its data flows, processing location, vendor security practices, and integration points—demand individual evaluation.
What happens if our Business Associate experiences a breach?
Your Business Associate must notify you of breaches involving your PHI. You’re then responsible for determining if the breach requires notification to affected individuals under HIPAA’s Breach Notification Rule. Business Associates bear liability for their own HIPAA violations, but you remain responsible for properly vetting vendors and maintaining oversight, so inadequate due diligence could result in shared liability.
Can we audit our Business Associates to verify HIPAA compliance?
Your BAA should include the right to audit Business Associates or receive third-party audit reports. For critical vendors handling significant PHI volumes, regular security assessments are prudent. Many cloud and SaaS providers offer SOC 2 reports or similar third-party attestations that provide insight into their security practices without requiring on-site audits.
How does HIPAA apply to AI-generated clinical documentation?
AI-generated clinical notes, summaries, or diagnostic suggestions become part of the patient’s medical record and must be protected like any other PHI. The healthcare provider remains responsible for accuracy and completeness regardless of AI assistance. Documentation should indicate when AI tools contributed to clinical records, and providers must review AI output for errors before including it in official patient documentation.
What security measures are most critical for HIPAA compliance with modern technology?
While comprehensive security requires many controls, prioritize encryption of PHI both in transit and at rest, multi-factor authentication for all system access, comprehensive audit logging and monitoring, regular employee security training, and thorough vendor management with appropriate BAAs. These foundational controls address the majority of breach scenarios and demonstrate basic HIPAA compliance commitment.
How Technijian Can Help
Maintaining HIPAA compliance while leveraging modern AI and cloud technologies requires specialized healthcare IT expertise that balances innovation with regulatory requirements. Technijian brings over two decades of experience securing healthcare data for medical practices throughout Orange County and Southern California.
Comprehensive HIPAA Compliance Services
Our healthcare IT specialists conduct thorough HIPAA compliance readiness assessments that examine your entire technology infrastructure. We identify vulnerabilities in your AI workflows, cloud deployments, and automated systems before they become compliance violations or security incidents. Our risk assessment methodology specifically addresses the unique challenges of modern healthcare technology, from machine learning platforms to virtual desktop environments.
We design security architectures that enable your practice to adopt cutting-edge AI diagnostics, cloud flexibility, and workflow automation without compromising patient data protection. Our implementations include HIPAA-compliant cloud VDI solutions with encrypted connections and multi-factor authentication, AI sandboxing environments that process data securely without creating compliance risks, automated compliance monitoring systems that continuously verify your security posture, and zero trust network architectures that segment PHI from general infrastructure.
Business Associate Management and Vendor Security
Managing the expanding ecosystem of healthcare technology vendors has become a full-time compliance challenge. Technijian reviews Business Associate Agreements to ensure they contain appropriate HIPAA provisions, conducts vendor security assessments before you commit to new platforms, maintains ongoing monitoring of Business Associate compliance, and documents your due diligence for audit purposes.
Our team stays current with OCR guidance and emerging healthcare technology regulations, ensuring your vendor relationships meet evolving compliance requirements. We help you navigate the complex shared responsibility model of cloud computing, clearly defining where provider obligations end and your responsibilities begin.
Employee Training and Security Awareness
We develop customized HIPAA training programs that address the specific AI tools, cloud systems, and workflows your organization uses. Our scenario-based training helps clinical staff, administrators, and IT personnel understand how compliance principles apply to their daily responsibilities. We conduct simulated phishing exercises, implement security awareness campaigns, and document training completion for audit purposes.
Incident Response and Breach Support
When security incidents occur, Technijian provides immediate response capabilities that contain breaches, preserve forensic evidence, and minimize PHI exposure. Our incident response services include 24/7 emergency support for suspected breaches, forensic investigation to determine incident scope and impact, breach notification assistance meeting HIPAA’s 60-day requirement, remediation implementation to prevent recurrence, and regulatory liaison support during OCR investigations.
We help you develop comprehensive incident response plans before breaches occur, including tabletop exercises that prepare your team for various scenarios involving AI system failures, cloud disruptions, and automation errors.
Ongoing Managed IT Security
HIPAA compliance isn’t a one-time project—it requires continuous monitoring, assessment, and adaptation as threats evolve and technologies change. Our managed IT services provide ongoing security monitoring with SIEM systems that detect suspicious activity, automated compliance scanning that identifies configuration drift, regular vulnerability assessments and patch management, backup and disaster recovery solutions protecting PHI availability, and endpoint protection across all devices accessing your systems.
Our managed services model means you have a dedicated healthcare IT partner monitoring your environment around the clock, providing expert guidance as you evaluate new technologies and helping you understand compliance implications before deployment decisions are finalized.
Why Southern California Healthcare Providers Choose Technijian
We’ve helped dozens of healthcare providers successfully adopt cloud technologies, implement AI tools, and automate administrative processes while maintaining strict HIPAA compliance. Unlike generic IT providers, we specialize in the healthcare sector’s specific compliance challenges. We speak the language of both technology and healthcare, translating complex regulatory requirements into practical implementation strategies.
Our local presence in Southern California means rapid on-site response when situations require it, combined with the sophisticated monitoring and automation capabilities of enterprise-scale managed services. We understand the operational realities of medical practices, from electronic health record workflows to patient scheduling systems, and design solutions that enhance rather than disrupt your clinical operations.
Get Your HIPAA Compliance Readiness Check
Are your AI tools, cloud infrastructure, and automated workflows properly secured for HIPAA compliance? Technijian’s comprehensive readiness assessment evaluates your current systems, identifies compliance gaps, and provides a clear remediation roadmap prioritized by risk.
Our assessment examines your complete healthcare IT environment including AI platforms and data flows, cloud hosting configurations and access controls, automation scripts and API security, employee training and security awareness, vendor relationships and Business Associate Agreements, incident response capabilities and breach procedures, and documentation completeness for audit readiness.
You’ll receive a detailed report outlining specific vulnerabilities, recommended remediation steps with timeline and resource requirements, estimated compliance gap closure costs, and ongoing monitoring recommendations to maintain your security posture.
Don’t wait for an OCR audit or security incident to discover compliance gaps. Contact Technijian today to schedule your HIPAA compliance readiness assessment. As a trusted managed IT services provider serving Orange County since 2000, we help healthcare organizations throughout Southern California navigate the complex intersection of advanced technology and regulatory compliance.
Reach out to our Irvine office or visit technijian.com to speak with a healthcare IT security specialist who understands the unique challenges facing medical practices in 2025. Protect your patients’ most sensitive information while confidently adopting the AI and cloud technologies that modern healthcare demands. Let Technijian be your partner in building a secure, compliant, and innovative healthcare IT infrastructure that supports your clinical mission while safeguarding the trust your patients place in you.
About Technijian
Technijian is a leading managed IT services provider founded in 2000 by Ravi Jain, dedicated to delivering comprehensive technology solutions to businesses across Orange County and Southern California. For over two decades, we have specialized in providing enterprise-grade IT infrastructure, cybersecurity, cloud services, and compliance solutions to organizations of all sizes.
Based in Irvine, California, our team of certified IT professionals brings deep expertise across multiple industries, with particular specialization in healthcare IT and HIPAA compliance. We understand the unique challenges facing medical practices, clinics, hospitals, and health services organizations as they navigate the complex intersection of advanced technology adoption and stringent regulatory requirements.
Our comprehensive service portfolio includes managed IT support and monitoring, cybersecurity solutions and threat protection, cloud migration and infrastructure management, Microsoft 365 deployment and optimization, backup and disaster recovery services, network design and implementation, and AI workflow automation consulting. We serve as a strategic technology partner, not just a service provider, helping organizations leverage innovation while maintaining security, compliance, and operational excellence.
Technijian’s commitment to staying at the forefront of technology trends means our clients benefit from cutting-edge solutions without the complexity of managing them independently. Our proactive approach to IT management prevents problems before they impact your operations, and our local Southern California presence ensures rapid response when you need us most.